162x Filetype PDF File size 1.08 MB Source: www.berkshirewestccg.nhs.uk
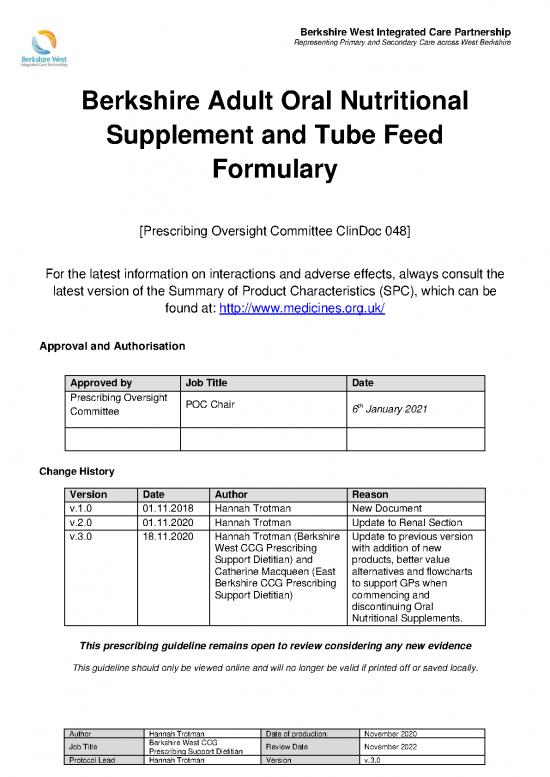
Berkshire West Integrated Care Partnership
Representing Primary and Secondary Care across West Berkshire
Berkshire Adult Oral Nutritional
Supplement and Tube Feed
Formulary
[Prescribing Oversight Committee ClinDoc 048]
For the latest information on interactions and adverse effects, always consult the
latest version of the Summary of Product Characteristics (SPC), which can be
found at: http://www.medicines.org.uk/
Approval and Authorisation
Approved by Job Title Date
Prescribing Oversight POC Chair
th
Committee 6 January 2021
Change History
Version Date Author Reason
v.1.0 01.11.2018 Hannah Trotman New Document
v.2.0 01.11.2020 Hannah Trotman Update to Renal Section
v.3.0 18.11.2020 Hannah Trotman (Berkshire Update to previous version
West CCG Prescribing with addition of new
Support Dietitian) and products, better value
Catherine Macqueen (East alternatives and flowcharts
Berkshire CCG Prescribing to support GPs when
Support Dietitian) commencing and
discontinuing Oral
Nutritional Supplements.
This prescribing guideline remains open to review considering any new evidence
This guideline should only be viewed online and will no longer be valid if printed off or saved locally.
Author Hannah Trotman Date of production: November 2020
Job Title Berkshire West CCG Review Date November 2022
Prescribing Support Dietitian
Protocol Lead Hannah Trotman Version v.3.0
2
Berkshire Adult Oral Nutritional Supplement and Tube Feed Formulary
Traffic Light Coding:
Green: Can be initiated by any prescriber when ACBS indicators for prescription of borderline substances are met (see page footer).
Amber: Should only be prescribed on the recommendation of a Dietitian or other specialist when ACBS indicator for prescription of borderline
substances are met– refer to their advice for quantity and duration of prescription.
▪ If further guidance on nutritional supplementation is required, the patient should be referred to a Dietitian for assessment.
▪ The products included in this formulary should be safe and suitable for most patients to use. Please refer to the BNF, manufacturer’s information or
Dietitian for advice if a patient is following a restricted diet for medical/religious purposes, or has complex nutritional needs.
▪ Dietitians should only use products listed on this formulary, as they have gone through CCG approval. If however a Dietitian requests a product not
included on the formulary for clinical reasons, they must inform the prescriber that it is non-formulary and give clear justification for its use.
▪ All prescriptions of Oral Nutritional Supplements should be reviewed every 3-6 months (or more frequently if there is a clinical need) as per NICE CG32
guidance. To assist in the management of this, please put ONS on ‘acute’ prescription and consider using ‘starter packs’ to provide a one week supply in a
variety of flavours, to help identify preference. Tube Feeds should remain on Repeat prescriptions.
▪ For patients who can make up a shake, Powder ONS are recommended first line as they are better value than bottled versions. Please see indication
column for guidance on the use of each product. Please note that products should only be used for the ACBS indicators they are specified for. Please see
the ACBS abbreviation key in the footer and other abbreviations on the final page. Please follow dietitian recommendations for monthly volumes.
▪ Allergens are listed as per BNF or from the product manufacturers before October 2020. It is the clinician’s responsibility to check each product for all
other allergens before prescribing. Products are gluten-free unless stated otherwise. N.B: Manufacturers state a product is ‘clinically lactose-free’, ‘lactose-
free’ or containing ‘residual lactose’ if the lactose content is below a certain threshold. This varies from <0.2g-1.0g per 100ml for different products.
▪ Many products on this formulary obtain Vitamin D from Lanolin (found in live sheep’s wool) which is not suitable for vegan diets, however may be accepted
in vegetarian diets. Some flavours (*) use cochineal as a colouring. If a patient follows a vegetarian or vegan diet, please check each product’s suitability.
Authors: Prescribing Support Dietitians - East Berkshire CCG, Berkshire West CCG Issue date:
Authorised by: Effective Prescribing & Performance Group and Area Prescribing Committee Review date: Version 3
▪ Abbreviations: FFM (Full Fat Milk), HP (High Protein), MCT (Multiple Chain Triglycerides) – see final page for further abbreviations.
▪ ACBS Indicators: Bowel Fistulae (BF), Continuous Ambulatory Peritoneal Dialysis (CAPD), Dysphagia (D), Disease-Related Malnutrition (DRM), Haemodialysis (HD), Proven Inflammatory
Bowel Disease (IBD), Intractable Malabsorption (IM), Pre-Operative preparation of undernourished patients (PO), Short Bowel Syndrome (SBS) and Total Gastrectomy (TG).
3
Pathway for Commencing Oral Nutritional Supplements (ONS) – Appendix 1
▪ Patients should have followed food first advice for at least one month if able to do so (see yellow boxᵡ), meet one of the ACBS indicators and
usually have a MUST score of 2 or above, in order to be eligible for ONS on NHS prescription.
▪ Screen patients for malnutrition using the MUST nutritional assessment tool, calculator found online: https://www.bapen.org.uk/screening-and-
must/must-calculator. Please follow Dietetic action plans as per below:
Patient identified as having a low BMI and/or unintentional weight loss
Complete MUST screening tool
MUST Score 2 or above
MUST Score 0 or 1 Provide high energy and protein food first
advice for patient/carer to follow for at least
one month (if able to do so ᵡ), resources:
Review MUST score in 3 months Review MUST score in 1 month
(MUST 1) or yearly (MUST 0)** ‘Making the most of what you eat’ and
‘Homemade fortified milkshake’ on DXS.*
OTC milkshakes/soups also available, for example ➢If weight has stabilised or improved:
Complan®, Meritene® or NutriVigor® Continue with food first advice and review MUST
Consider investigations for weight loss. score every 1-3 months**
If MUST score remains less than 2,
continue with food first advice and If weight deteriorates and MUST score becomes ➢If patient unable to follow food first advice (see
review every 3-12 months 2 or above, OR patient is unable to do food first, belowᵡ) OR weight has deteriorated despite food
depending on clinical judgement. follow guidance for MUST 2+ in red boxes. first, plus patient meets an ACBS indication listed for
the specific product,*** consider starting ONS as
per formulary. Patients with a MUST score of 2+ can
* Please refer to the dietitians if patient has special requirements e.g. dysphagia or requires a milk-free diet. be referred to the Community Dietitians.
** MUST score can be repeated more frequently if concerned.
***ACBS Criteria: short bowel syndrome, dysphagia, intractable malabsorption, pre-operative preparation of
undernourished patients, proven inflammatory bowel disease, total gastrectomy, bowel fistulae, disease- ᵡ Some patients may not be able to follow food first
related malnutrition, continuous ambulatory peritoneal dialysis (CAPD) and haemodialysis. advice, for example: due to suspected upper GI cancer,
severe frailty, renal disease or on the advice of Dietitian.
Please check each product’s specific ACBS criteria.
▪ Abbreviations: FFM (Full Fat Milk), HP (High Protein), MCT (Multiple Chain Triglycerides) – see final page for further abbreviations.
▪ ACBS Indicators: Bowel Fistulae (BF), Continuous Ambulatory Peritoneal Dialysis (CAPD), Dysphagia (D), Disease-Related Malnutrition (DRM), Haemodialysis (HD), Proven Inflammatory
Bowel Disease (IBD), Intractable Malabsorption (IM), Pre-Operative preparation of undernourished patients (PO), Short Bowel Syndrome (SBS) and Total Gastrectomy (TG).
4
Pathway for the Discontinuation of Oral Nutritional Supplements (ONS) – Appendix 1
CRITERIA: Patient has been prescribed ONS for ≥6-12 months and is not currently under a Dietitian
Check MUST score using BAPEN MUST calculator
https://www.bapen.org.uk/screening-and-must/must-calculator
MUST Score 0 or 1 and/or MUST Score 2 or above and/or
patient doesn’t meet ACBS patient meets ACBS indicator.
indicator (see page footer).
Provide high energy and protein food
first advice for patient/carer to follow Yes Has patient had previous No
STOP ONS prescription* and
for at least one month dietetic input?
explain that patient no longer ** ∆
(where able to do so ), resources :
meets ONS prescribing criteria
‘Making the most of what you eat’
(unless weight is deteriorating towards •Has weight been stable for ≥3-6 Consider referring to
and ‘Homemade fortified milkshake’, months OR is weight ‘normal’ or at
MUST 2, then monitor and review). Dietitians via health
also found on DXS. baseline for patient?
OTC milkshakes/soups also available, for hub for support, or
• Have agreed dietetic goals been met?
exampleComplan®, Meritene® or Nutrivigor® undertake review
Review MUST SCORE:
• Is patient managing to eat their using red flowchart
• MUST 0: 1 year normal diet and is gaining weight? on left.
• MUST 1: 3 months’ time
∆
Provide food first advice and advise Yes No
OR more frequently if clinical concern.
patient to contact GP if deterioration in
Consider weaning ∆
If patient’s malnutrition risk increases, weight. Review progress in Reiterate food first advice and check
follow red pathway on right. off ONS* patient is taking prescribed dose i.e.
1-3 months depending on risk.
BD, and doing food first interventions
alongside ONS. Consider dietetic
* ONS can be weaned off by, for example, reducing to OD for 1 month then stopping if patient remains stable. If patient is not
**
taking prescribed therapeutic dose i.e. BD or is taking ONS sporadically, discontinue prescription and advise food first. review if patient has complex needs.
** Some patients may not be able to follow food first advice, for example: due to suspected upper GI cancer, severe frailty, renal
disease or those without care support. Review progress in 1-3 months (depending
This flowchart is to be used only as a guide. Please use your own clinical judgement and contact the dietitians if further support on risk) and repeat above steps.
required or patient has complex needs i.e. Dysphagia, Dementia or ONS is sole source of nutrition.
▪ Abbreviations: FFM (Full Fat Milk), HP (High Protein), MCT (Multiple Chain Triglycerides) – see final page for further abbreviations.
▪ ACBS Indicators: Bowel Fistulae (BF), Continuous Ambulatory Peritoneal Dialysis (CAPD), Dysphagia (D), Disease-Related Malnutrition (DRM), Haemodialysis (HD), Proven Inflammatory
Bowel Disease (IBD), Intractable Malabsorption (IM), Pre-Operative preparation of undernourished patients (PO), Short Bowel Syndrome (SBS) and Total Gastrectomy (TG).
no reviews yet
Please Login to review.